Retina
What is Diabetic Retinopathy?
Diabetic retinopathy, also known as diabetic eye disease, is the most common cause of vision loss among people with diabetes. The condition affects the retina, a small patch of tissue at the back of the eye. The retina turns rays of light into signals for the brain, which allows us to see. A healthy retina is essential to good vision — any amount of retinal damage can cause irreversible vision loss.
There are four stages of diabetic retinopathy:
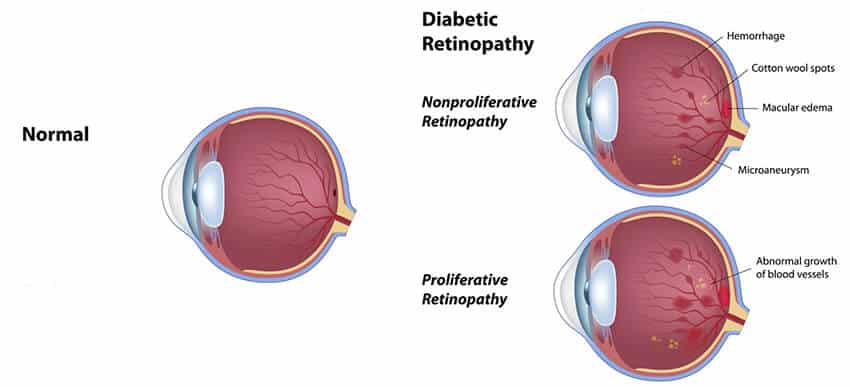
What causes diabetic retinopathy?
High blood sugar levels cause damage to the tiny blood vessels in the retina of diabetic patients. Over time, the blood vessels start to swell and leak blood into the eye, which causes blind spots and blurry vision. The blood vessels can also close completely, which blocks the passage of blood to parts of the eye.

What are the symptoms?
Diabetic retinopathy is not detectable in its early stages, as there are typically no symptoms. In most cases, the eye disease will progress unnoticed by the patient until they experience blurry vision or “floaters,” which appear as dark spots in your line of sight. A comprehensive eye exam is required in order to examine the blood vessels of the retina and diagnose diabetic retinopathy. If vision has already been affected by the leakage of fluid in the retina, prompt treatment is required in order to prevent permanent vision loss.
Can you prevent diabetic retinopathy?
Anyone with type 1 or type 2 diabetes is at risk of developing diabetic retinopathy. 45 percent of diabetic Americans experience some stage of diabetic retinopathy, while only half of those people are aware they have the disease.
If you have diabetes, the best way to reduce your risk of diabetic retinopathy is to control your blood sugar levels, take medications as prescribed, stay active, and eat healthy. People with diabetes should also visit an eye doctor for a comprehensive dilated eye exam at least once a year. Early detection and treatment of diabetic retinopathy can help protect against long-term eye problems and vision loss.
Diabetic Retinopathy Treatment Options
In most cases, vision loss due to diabetic retinopathy is irreversible. The swelling of blood vessels in the retina can, however, be treated a number of different ways.
Treatment for diabetic macular edema and PDR includes:
Macular Degeneration
Age-related macular degeneration (AMD) is a common eye disease associated with aging that gradually destroys sharp, central vision. It is one of the leading causes of legal blindness and vision impairment in older Americans.
The progression of AMD can be slow or rapid, but the deterioration of central vision generally occurs over a period of a few years.
If you experience the following, see your Eye M.D. right away:
- Straight lines appear wavy
- Difficulty seeing at a distance
- Decreased ability to distinguish colors
- Inability to see details, such as faces or words in a book
- Dark or empty spots block the center of your vision
Although the exact cause of macular degeneration is unknown, several studies have shown the following individuals may be at risk:
- People over age 60
- People with hypertension
- People that smoke
- People with a family history of AMD

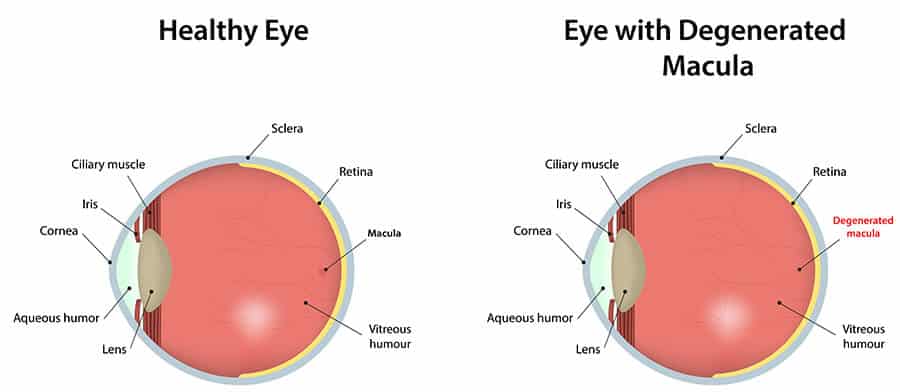
The “dry” form of macular degeneration affects approximately 90 percent of those with AMD. Studies have found that high levels of zinc and antioxidants play a key role in slowing the progression of dry macular degeneration in advanced cases.
The “wet” form affects only 10 percent of those with AMD, but it accounts for 90 percent of all severe vision loss from the disease. For these individuals, conventional laser treatment and photodynamic therapy (PDT) treatment is used. PDT is used to reduce the risk of moderate to severe vision loss in patients with a few very specific forms of “wet” macular degeneration. Other experimental treatments that are being investigated include, intraocular antineovascular injections and the insertion of a “retinal chip” to restore vision loss.
Early detection and treatment is the best defense against losing your vision. If you are at risk for macular degeneration, see your eye doctor for a complete eye exam at least every one to two years. If your vision has been reduced, low vision rehabilitation resources can help you maintain an excellent quality of life.
Please call 815-485-2727 or make an appointment online.

